Fertility

Aaditya Fertility & Women Care Center provides infertility services such as:
- IUI (AIH/AID)
- IVF
- ICSI
- Surgical Sperm Retrieval
- Oocyte Retrieval
- Embryo Transfer
- Frozen Embryo Transfer
- Surrogacy
AIH (Artificial Insemination with Husband's Sperm)

For a woman to get pregnant, a man’s sperm must travel from the vagina through the cervix (narrow, lower part of the womb), into the uterus (womb), and up into one of the fallopian tubes. If sperm arrives in the tubes soon after the release of the egg from the ovary (ovulation), the sperm and egg can meet in the tube, most commonly, on the side that ovulation took place, and then fertilization may occur.
 Because the cervix naturally limits the number of sperm that enter the uterus, only a few sperm actually make their way to the fallopian tubes. Intrauterine insemination (IUI) is a procedure that bypasses the cervix and places sperm into a woman’s uterus around the time of ovulation. Placing the sperm directly into the uterus makes the trip to the fallopian tubes much shorter. This way, there is a better chance that more sperm will make their way closer to the egg. This procedure is performed to improve a woman’s chance of getting pregnant.
Because the cervix naturally limits the number of sperm that enter the uterus, only a few sperm actually make their way to the fallopian tubes. Intrauterine insemination (IUI) is a procedure that bypasses the cervix and places sperm into a woman’s uterus around the time of ovulation. Placing the sperm directly into the uterus makes the trip to the fallopian tubes much shorter. This way, there is a better chance that more sperm will make their way closer to the egg. This procedure is performed to improve a woman’s chance of getting pregnant.
Female infertility
 Women who do not release an egg regularly (ovulate) may take medications to help them ovulate regularly. These women may need IUI to time insemination at about the same time as ovulation. Also, IUI is helpful when a woman’s cervix has scarring that prevents the sperm from entering the uterus from the vagina. This may be seen in women who have had surgery on their cervix (cryosurgery, cone biopsy, LEEP, etc.).
Women who do not release an egg regularly (ovulate) may take medications to help them ovulate regularly. These women may need IUI to time insemination at about the same time as ovulation. Also, IUI is helpful when a woman’s cervix has scarring that prevents the sperm from entering the uterus from the vagina. This may be seen in women who have had surgery on their cervix (cryosurgery, cone biopsy, LEEP, etc.).
Infertile women sometimes take medications (by mouth or as an injection) that cause their ovaries to produce several eggs at once. These women appear to have a better chance of getting pregnant if they also have IUI.
Male infertility
 IUI is most commonly used when the male partner has a low sperm count or if the movement of the sperm (motility) is less than ideal. But also, IUI is useful for couples who are infertile because the male has problems developing an erection or being able to ejaculate. For example, retrograde ejaculation is when the sperm are released backwards into the bladder, instead of through the penis, at the time of male orgasm. A number of medical conditions can cause retrograde ejaculation. Sperm ejaculated into the bladder can be taken from urine and used for IUI. Also, IUI may help if the man has an abnormal urethral opening (opening of the penis).
IUI is most commonly used when the male partner has a low sperm count or if the movement of the sperm (motility) is less than ideal. But also, IUI is useful for couples who are infertile because the male has problems developing an erection or being able to ejaculate. For example, retrograde ejaculation is when the sperm are released backwards into the bladder, instead of through the penis, at the time of male orgasm. A number of medical conditions can cause retrograde ejaculation. Sperm ejaculated into the bladder can be taken from urine and used for IUI. Also, IUI may help if the man has an abnormal urethral opening (opening of the penis).
AID (Artificial Insemination with Donor Sperm)
 Artificial insemination with donor sperm consists of placing sperm obtained from a sperm bank inside the uterus. These sperm donors are tested for infectious deseases and quarantined for six months. Artificial insemination with donor sperm is recommended when the partner has some kind of hereditary disease or his testicles are unable to produce sperms (testicular failure).
Artificial insemination with donor sperm consists of placing sperm obtained from a sperm bank inside the uterus. These sperm donors are tested for infectious deseases and quarantined for six months. Artificial insemination with donor sperm is recommended when the partner has some kind of hereditary disease or his testicles are unable to produce sperms (testicular failure).
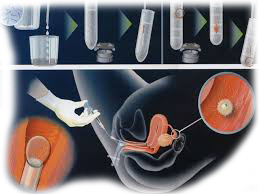
How is IUI done?
 Once collected, the semen sample is then “washed” in the laboratory, to concentrate the sperm and remove the seminal fluid (seminal fluid can cause severe cramping in the woman). This process can take up to two hours to complete.
Once collected, the semen sample is then “washed” in the laboratory, to concentrate the sperm and remove the seminal fluid (seminal fluid can cause severe cramping in the woman). This process can take up to two hours to complete.
IUI is performed near the time that the female partner is ovulating. The IUI procedure is relatively simple and only takes a few minutes. The woman lies on an examining table and the clinician inserts a speculum into her vagina to see her cervix. A catheter (narrow tube) is inserted through the cervix into the uterus and the washed semen sample is slowly injected.
In Vitro Fertilization (IVF)
 In vitro fertilization (IVF) is a method of assisted reproduction that involves combining an egg with sperm in a laboratory dish. If the egg fertilizes and begins cell division, the resulting embryo is transferred into the woman’s uterus where it will hopefully implant in the uterine lining and further develop. IVF bypasses the fallopian tubes and is usually the treatment of choice for women who have badly damaged or absent tubes.
In vitro fertilization (IVF) is a method of assisted reproduction that involves combining an egg with sperm in a laboratory dish. If the egg fertilizes and begins cell division, the resulting embryo is transferred into the woman’s uterus where it will hopefully implant in the uterine lining and further develop. IVF bypasses the fallopian tubes and is usually the treatment of choice for women who have badly damaged or absent tubes.
Intracytoplasmic Sperm Injection (ICSI)
Before a man's sperm can fertilize a woman's egg, the head of the sperm has to attach to the outside of the egg. Then it pushes through the outer layer of the egg to the inside of the egg (cytoplasm). Sometimes the sperm cannot penetrate the outer layer. A procedure called intracytoplasmic sperm injection (ICSI) can help fertilize the egg by injecting the sperm directly into the egg.
How does ICSI work?
In ICSI, a single sperm is injected into the cytoplasm of the ovum to effect fertilization. The fertilized egg grows in the laboratory in a special medium, for one to five days, then it is placed in the woman's uterus (womb).
Why would I need ICSI?

ICSI helps to overcome a man's fertility problem, for instance:
- He may produce too few sperm
- His sperm may not be shaped correctly or move in a normal fashion
- The sperm may have trouble attaching to the egg
- A blockage in his reproductive tract may keep sperm from getting out
ICSI can also be used when the use of traditional IVF has not produced fertilization, regardless of the condition of the sperm.
Will ICSI work?
ICSI fertilizes 50% to 80% of eggs. But the following may occur after the use of ICSI:
- The ICSI procedure might damage some eggs
- The egg might not grow into an embryo even after it is injected with sperm
- The embryo may stop growing
Once fertilization takes place, a couple's chance of giving birth to a single baby, twins, or triplets is the same as IVF.
Sperm Retrieval Techniques
These techniques are offered for males who have sperms absent in their semen sample due to obstruction in the reproductive tract. PESA/TESA/TESE are procedures in which sperms can be removed from the epididymis or the testis and used for fertilization by ICSI.
Percutaneous Epididymal Sperm Aspiration (PESA)
 Percutaneous epididymal sperm aspiration (PESA) is a sperm aspiration procedure in which a needle is inserted into the epididymis (gland that carries sperm from testicle to vas deferens) in order to retrieve sperms for ICSI.
Percutaneous epididymal sperm aspiration (PESA) is a sperm aspiration procedure in which a needle is inserted into the epididymis (gland that carries sperm from testicle to vas deferens) in order to retrieve sperms for ICSI.
Testicular Sperm Extraction (TESE)
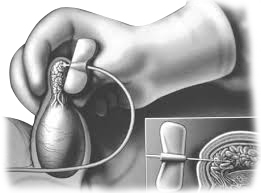 Testicular Sperm Extraction (TESE) is the operative removal of testicular tissue in an attempt to collect living sperms for use in ICSI.
Testicular Sperm Extraction (TESE) is the operative removal of testicular tissue in an attempt to collect living sperms for use in ICSI.
Testicular Sperm Aspiration(TESA)
Testicular Sperm Aspiration is a sperm aspiration procedure in which a fine needle is used to aspirate some of the testicular tubules that contain live sperms under suction, which can be used for ICSI.
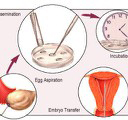
Embryo Transfer

Embryo Transfer is a procedure in which the fertilized egg is transferred into the uterus of the woman. The objective of embryo transfer is to facilitate conception following fertilisation from in-vitro fertilisation procedure.
Depending on your situation between one and three of the best quality embryos are selected and then transferred to the woman's womb. An embryo must successfully attach itself to the wall of the womb for pregnancy to begin.
Frozen Embryo Transfer
Frozen / Thawed embryo transfer is a treatment that involves implanting embryos that were retrieved from the patient during previous IVF cycle and held safely in a frozen state.
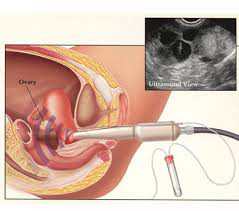
Oocyte Retrieval

Oocyte retrieval is the process of collecting mature eggs directly from the women's ovaries prior to their release from ovarian follicles.
Oocyte retrieval is a minor surgical procedure which takes only 15-30 minutes. It is usually performed while the woman is unconscious under short general anaesthesia. Ova are collected by inserting a fine needle through the woman's vagina into the ovaries using ultrasound guidance.
The collection of mature oocytes is a prerequisite for IVF and other ART procedures.
Cryopreservation

Sperm Freezing
Some men are diagnosed with an illness whose treatment may have an adverse effect on their sperms and/or their count. They may feel disappointed for not being able to start or complete their family. Now, there is an option available to preserve their sperms by freezing. Also men may collect and freeze (cryopreserve) their sperm for future use before having a vasectomy, testicular surgery, or radiation/chemotherapy treatment for cancer. The sperm can then be used later for ART procedures.
Vitrification
 Vitrification is an advanced cell freeing technique, which allows a higher survival rate after thawing due to the fact that high concentration of cryoprotectors are used along with reduced volumes and timings. Thus the formation of intracellular ice crystals is prevented.
Vitrification is an advanced cell freeing technique, which allows a higher survival rate after thawing due to the fact that high concentration of cryoprotectors are used along with reduced volumes and timings. Thus the formation of intracellular ice crystals is prevented.
The vitrification process is used to freeze oocytes or embryos and it guarantees a survival rate of more than 80%.
This technique enables the vitrified oocytes which have survived the thawing process to have similar attributes to fresh ones. They are then able to be fertilized by the spermatozoids. The generated embryos can then be implanted and develop into healthy fetuses.
Oocyte donation (OD) or embryo donation (ED)
 Oocyte donation would necessitate using the husband's semen for fertilization and transferring the resultant embryo to the infertile female partner. Embryo donation would obviate the necessity of using the husband's semen. The choice of oocytes and embryos for oocyte or embryo donation would depend entirely on the circumstances prevalent at the time the infertile couple comes for treatment, and the access of the infertility clinic to frozen oocytes or embryos.
Oocyte donation would necessitate using the husband's semen for fertilization and transferring the resultant embryo to the infertile female partner. Embryo donation would obviate the necessity of using the husband's semen. The choice of oocytes and embryos for oocyte or embryo donation would depend entirely on the circumstances prevalent at the time the infertile couple comes for treatment, and the access of the infertility clinic to frozen oocytes or embryos.
Indications for oocyte or embryo donation
- . Gonadal dysgenesis
- . Pemature ovarian failure
- . Iatrogenic (due to ovarian surgery, radiation or chemical castration) ovarian failure.
- . Women who have resistant polycystic ovarian syndrome or who are poor responders to ovulation induction.
- . Women who are carriers of recessive autosomal disorders
- . Women who have attained menopause
Surrogacy
 Surrogacy is an arrangement in which a woman carries and delivers a child for another couple. The surrogate may be the child's genetic mother called traditional surrogacy (partial surrogacy). She may be genetically unrelated to the child called gestational surrogacy (full surrogacy).
Surrogacy is an arrangement in which a woman carries and delivers a child for another couple. The surrogate may be the child's genetic mother called traditional surrogacy (partial surrogacy). She may be genetically unrelated to the child called gestational surrogacy (full surrogacy).
Surrogacy may be appropriate if the medical condition makes it impossible or dangerous to get pregnant and to give birth .
You require surrogacy if there is :
1. Absence or malformation of the womb
2. Repeated IVF implantation failure